InsideAssist
AI-Powered Claims Management Built for Dental Revenue Cycle Teams
InsideAssist automates claims follow-up, denial tracking, and EOB retrieval, allowing your team to focus on resolving unpaid claims instead of chasing them.
Contact Us Today! - 855-777-0801 - info@insidedesk.com
InsideAssist
InsideAssist automates claims follow-up, denial tracking, and EOB retrieval, allowing your team to focus on resolving unpaid claims instead of chasing them.
TRUSTED BY THE FASTEST-GROWING AND LEADING DSOS


























RCM teams spend countless hours logging into payer portals, chasing down statuses, and managing denials in spreadsheets. InsideAssist centralizes and automates these tasks, giving your team visibility, speed, and control at scale.
Save hours daily by automating claim status checks and EOB retrieval
Reduce denial-related delays by surfacing issues early
Track team performance and claim outcomes
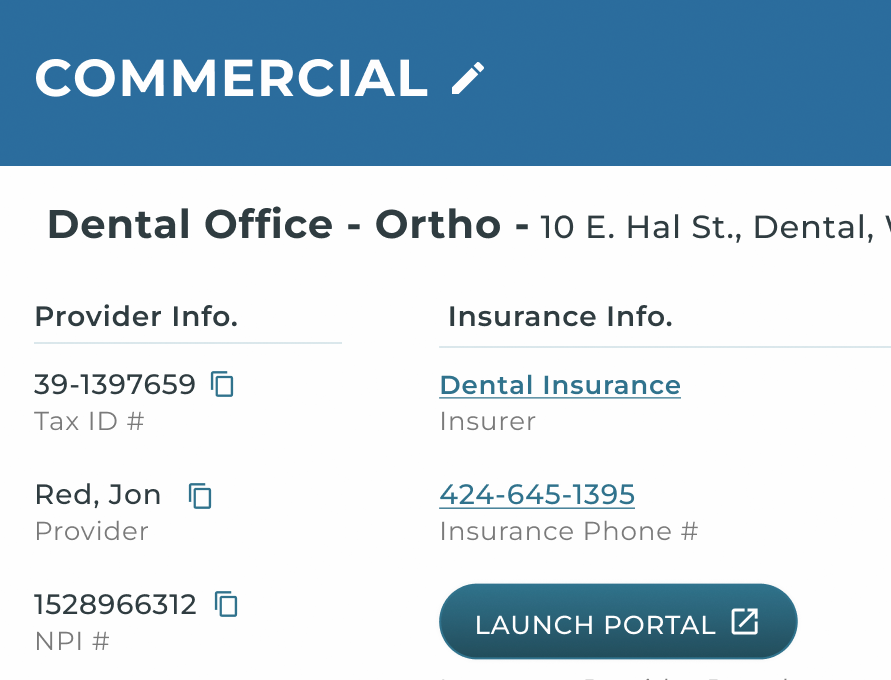
Cut down on the time spent logging into portals, now status checks are automatic.
AI helps your team focus on the claims that need attention. Automated EOBs for supported payers.
Know what’s going wrong and fix it before it happens again.
Get a clear view of team productivity and claim performance.
Payer responses, claim history, and daily priorities—organized and easy to use.
Automatically pull every new claim from your PMS and every major payer portal, so your data is always fresh when the team logs in.
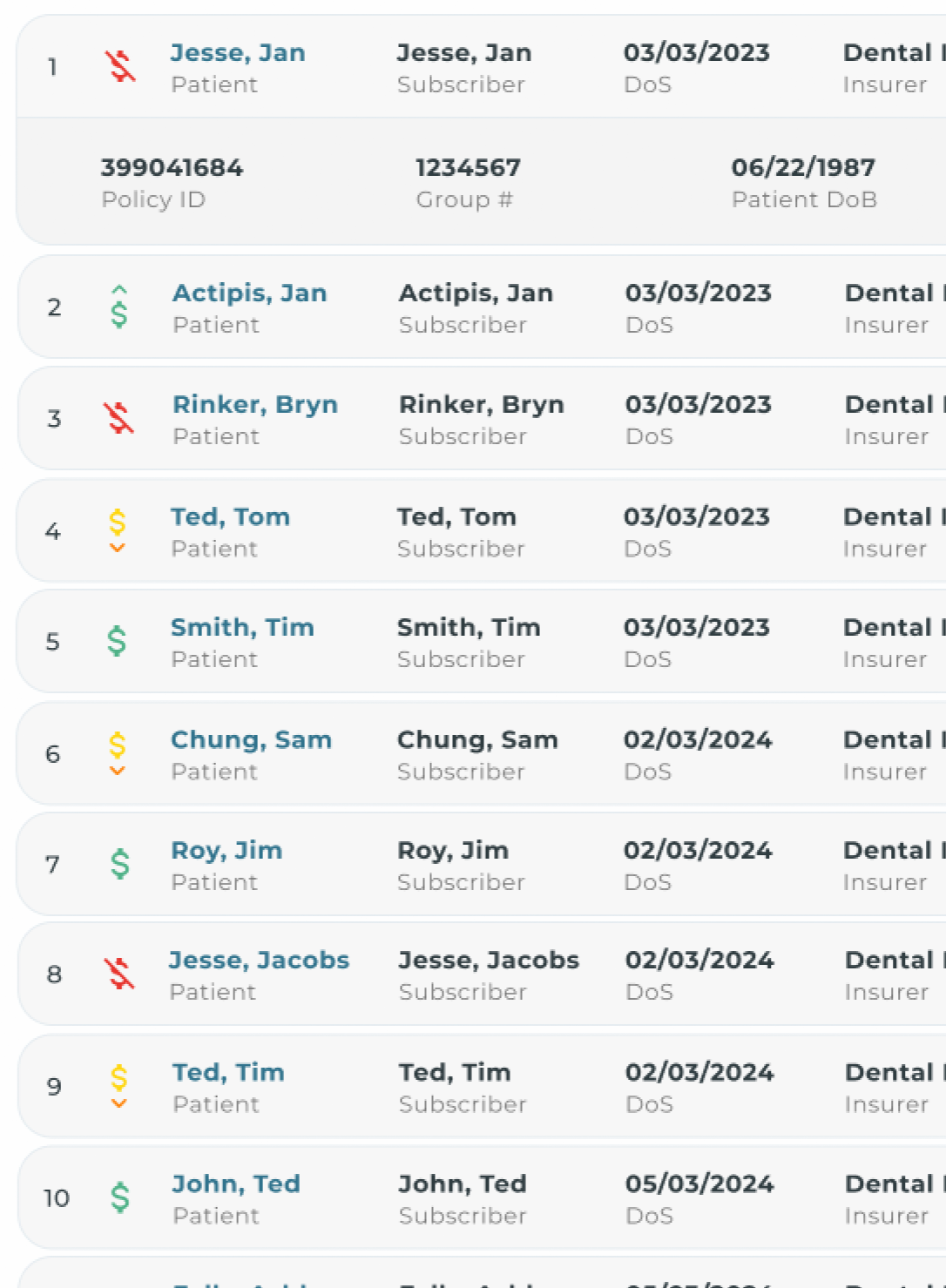
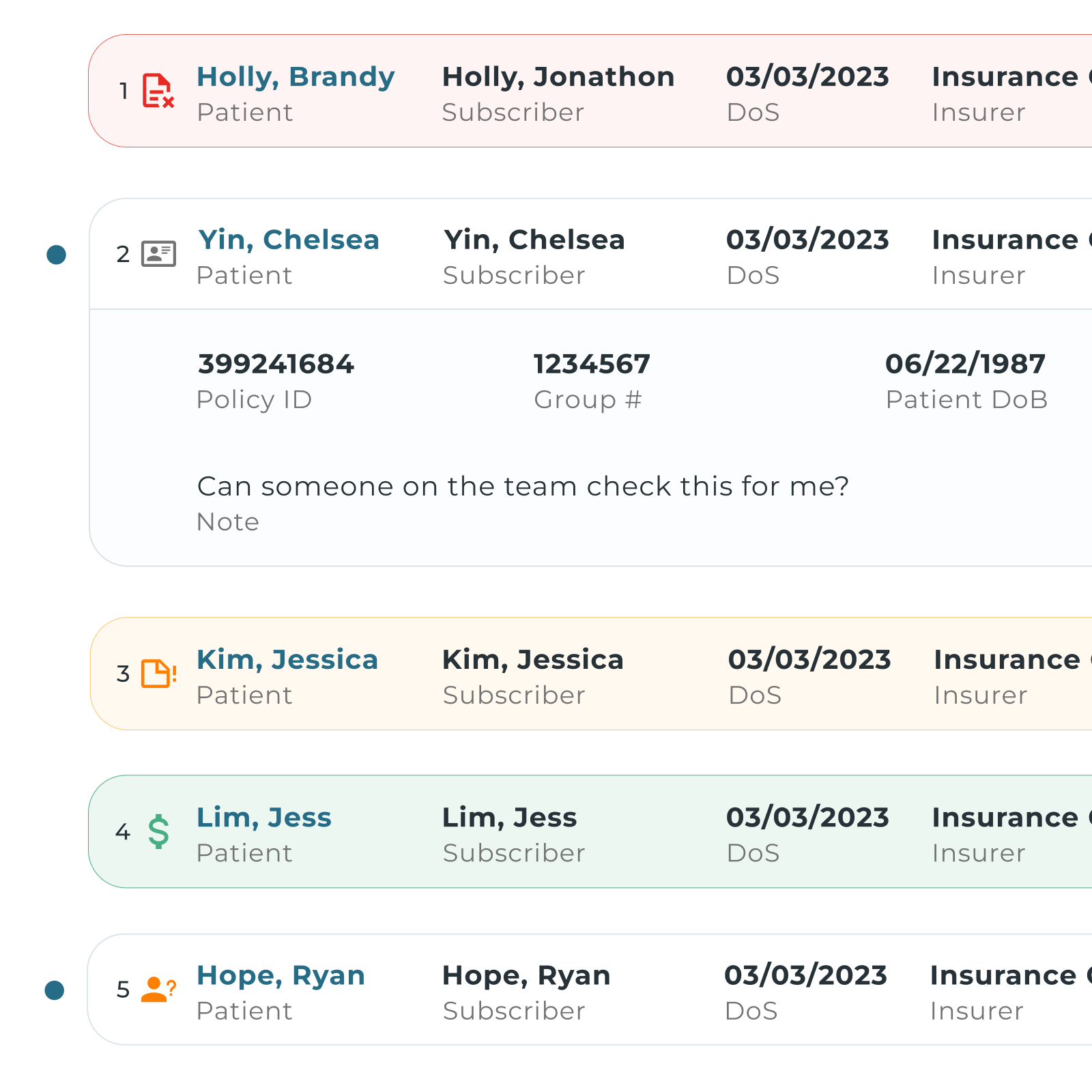
Categorize your claims into different buckets to help your team prioritize.
If a claim is still missing after a few days, InsideAssist flags it with clear icons that point to likely causes
The moment a resubmitted claim shows up on a portal, we move it from Issues to EOB, match expected vs. actual payment, and highlight any shortfalls
Open any claim to see patient details, code-level breakdowns, and EOB. Dashboards track productivity gains, days-to-payment, and revenue recovered, turning workflow wins into ROI.
Automatically pulls the latest claim statuses from your PMS and payer portals.
Retrieves and stores EOBs directly from payer portals, giving your team access to payment details, denial reasons and codes.
Surface and prioritize claim issues before they age. Use AI to group claims by status: denied, pending, paid, or underpaid.
View code-level payments, adjustments, and insurer notes pulled straight from the EOB for full transparency.
Provide a live aging report that allows you to filter claims by office, user role, or status, making it easy to prioritize the day’s work across teams.
Works seamlessly with your existing PMS, requiring no changes to your workflow. Data integrates with Power BI or your existing reporting suite.

"You solved half the battle…being able to automate EOB collection accurately and provide the claim status. I think it’s awesome not only from a workflow standpoint, but an efficient one for my staff too. It’s always easier when you put things in one place, and you don’t have to jump around into a million different portals.”

Growth in 3 months
Active Users